Hey interop fam, today’s the day for a rant and some raw and unadulterated metaphor. I’ll take you on a ride as we explore why legacy standards are so damn hard to get rid of and how regulation can help (but only if wielded correctly). Buckle up.
⚠️ Brief Interlude ⚠️
Before we dive in, a small life update: I’ve moved over to Zeus Health, ̶a̶ ̶̶̶̶̶̶̶v̶̶̶̶̶̶̶i̶̶̶̶̶̶̶r̶̶̶̶̶̶̶t̶̶̶̶̶̶̶u̶̶̶̶̶̶̶a̶̶̶̶̶̶̶l̶̶̶̶̶̶̶ ̶̶̶̶̶̶̶f̶̶̶̶̶̶̶i̶̶̶̶̶̶̶r̶̶̶̶̶̶̶s̶̶̶̶̶̶̶t̶̶̶̶̶̶̶ ̶̶̶̶̶̶̶c̶̶̶̶̶̶̶a̶̶̶̶̶̶̶r̶̶̶̶̶̶̶e̶̶̶̶̶̶̶ ̶̶̶̶̶̶̶c̶̶̶̶̶̶̶o̶̶̶̶̶̶̶m̶̶̶̶̶̶̶p̶̶̶̶̶̶̶a̶̶̶̶̶̶̶n̶̶̶̶̶̶̶y̶̶̶̶̶̶̶ ̶̶̶̶̶̶̶f̶̶̶̶̶̶̶o̶̶̶̶̶̶̶r̶̶̶̶̶̶̶ ̶̶̶̶̶̶̶t̶̶̶h̶̶̶e̶̶̶ ̶̶̶G̶̶̶r̶̶̶e̶̶̶e̶̶̶k̶̶̶ ̶̶̶G̶̶̶o̶̶̶d̶̶̶ ̶̶̶c̶o̶̶̶m̶̶̶m̶̶̶u̶̶̶n̶̶̶i̶̶̶t̶̶̶y̶̶̶… ̶a̶n̶ ̶i̶n̶d̶u̶s̶t̶r̶i̶a̶l̶ ̶s̶t̶r̶e̶n̶g̶t̶h̶ ̶a̶p̶h̶r̶o̶d̶i̶s̶i̶a̶c̶ ̶t̶e̶l̶e̶p̶r̶e̶s̶c̶r̶i̶b̶e̶r̶… an early stage startup focused on accelerating digital health builders with a platform of healthcare-oriented, API-first services. It’s really exciting! Some might say a rocket ship. And we are hiring engineers, so please hit me up or apply if at all interested. Or, if you like my writing, just apply so that I can continue to have a job, which funds this side endeavor.
A Mini MBA For Standards
As we’ve mentioned before, standards are products. They are a product of consensus, which is sweet, but that alone does not predestine their adoption or victory. Standards win in some cases, but may lose to other standards or proprietary products. And as a result, the principles that apply to regular products in different markets also apply to standards! But, in this case, the markets may actually be entire countries.
When a market has a problem, but no solution, it’s “white space” or “greenfield” and ripe for quick adoption. It is, as the experts say, like shooting fish in a barrel, assuming you’ve got the right gun and barrel’s location.
When a market has a problem, but has adopted an existing solution that’s on the market, these incumbent solutions can be difficult to displace. Several of the “7 Powers” can protect this incumbent:
Given the large customer base, there are economies of scale often in play - the cost is spread over a larger number of users.
Tech’s favorite moat, network effects, often come with scale - strongly if the product is a platform or marketplace, for sure, but almost all products have some weak network effects at scale through social elements like language, belief, or, in the case of Gen Z, whatever vibes are.
Products in saturated markets almost always have high switching costs - this is a biggie in terms of preventing the adoption of new technology. You may hate Jira for product management or Salesforce for CRM or Epic/Cerner for EHR, but hell, you certainly don’t want to go through the rigors of implementing a new product again, trying to transfer your data, knowing there will be some lossiness in that data transfer, and the abject pain of users learning that new software.
Sometimes that market leader has a cornered resource that is nigh impossible to disrupt or overcome - regulatory capture. A better product cannot be used when the existing one has a government mandate. NCPDP’s selection as a standard largely had to do with its constituency’s ability to lobby, not its value as a superior standard (more on this later).
These dynamics are what make capitalism so gosh darn fun and act as fodder for any number ofBen Thompson orNot Boring Substack lookalikes and endless discourse in business and tech Twitter.
Banning the Fax
*record scratch*
*freeze frame*
Yup, that’s me above. You're probably wondering how I ended up in this situation, writing an article about business topics I self-admittedly have only passively accumulated by osmosis from better educated colleagues and transitive property from my Wharton twin brother (little known fact, twins can share knowledge like that and it’s a very underrated superpower).
It all started with an article concerning healthcare in the Netherlands, my previous home across the Atlantic and the land of bitterballen (elite snack food), stroopwaffels, and windmills.
Posted by Herko Coomans, the International Digital Health Coordinator for the Dutch and an absolute legend in health IT, it’s (obviously) in Dutch, but if you Google Translate it, you can see that the new law is pushing the mandatory use of electronic forms of exchange when it comes to health information. This means no more fax of your records to your PCP, no more DVDs of lackluster quality for your MRI, and no more printouts to carry to your reference lab.
This is amazing, but simultaneously infuriating:
Amazing, because the future envisioned is what everyone wants, both in the Netherlands and here.
Infuriating, because I selfishly also want the nice things for us here domestically.
The approach is undoubtedly disruptive and heavy-handed. Hospitals and their software vendors will have to scramble to determine how to replace each and every workflow with an electronic version. There will be pain in this transition. There will be pushback in this transition. There will (almost certainly) be substantial delays in this transition.
But it’s also, in my frank and “too many coffees on a Saturday morning”-fueled opinion, the right one. This goes back to those business principles I butchered to start the article. Fax is a ubiquitous technology that has saturated many niche segments of the healthcare market. Displacing it is tough! The same goes for many other legacy standards - DVD, paper, HL7v2, you name it. Things stick around well past their due date.


Crossing the Chasm
“But wait, Brendan,” you might say, “domestically we’ve shown some appetite for mandating the use of certain standards - X12, NCPDP, Direct, and now USCDI FHIR - for specific use cases. How is this any different?”
Thank you for asking, my imaginary straw man counterpart. The key aspect here is that you cannot just add a new product to the market and assume it will reach ubiquitous adoption. We can use that product parallel to understand why. In Geoffrey A. Moore’s Crossing the Chasm, the life cycle of production adoption is described as a curve with a distinct chasm between “early market” and “mainstream market”.
We can apply this conceptually to national adoption as a country of different technologies. For instance, fax is an existing “product” that is the incumbent. It’s adopted across all of healthcare, for a variety of workflows and use cases. There are significant switching costs (the fax replacement has a price tag) and there’s certainly a network effect (when I know that I can fax to almost anyone, that’s superior to technologies that are less pervasive).
Direct Messaging is a technology allowing for electronic transfer of health information securely via SMTP, the same technology you use for email (with certified Health Information Service Providers who ensure only good actors are allowed into the ecosystem). Meaningful Use 2 mandated that EHR systems support it, so it’s pretty ubiquitous in the sense you’re hard pressed to find a system that doesn’t have on paper support for it.

Why, then, does fax still exist in America, if a superior electronic technology (product) has been brought to market and has regulatory incentive?
Simply put, Direct Messaging has not crossed the chasm for all current fax use cases. The regulatory adoption really only mandated it was fully supported for a single use case (pushing a continuity of care document), but not for all use cases (sending a photo, sending a referral, etc).
To push through and disrupt the “mainstream market” of most use cases across chasm, the new product needs to overcome the reservations of the early majority without the benefit of regulatory incentives. The moats we mentioned earlier protect that incumbent. For fax, there are switching costs, in that getting the software either from your EHR vendor or another supplier will cost money. Why fix what’s not (that) broken? More importantly, though, fax has a large network effect, in that you can reliably assume healthcare organizations still have one and that it can be used for all of your use cases.
Normally, in the private markets, this is a hard process requiring deft leadership and intense focus for a tech company with a regular product - attacking niche segments of the market underserved by the legacy technology to build up references and expanding from that point. In the case of DVD, Netflix artfully did this - pairing streaming with DVD mailing and iterating and improving their service until DVD is all but eliminated.
But when it comes to standards of exchange as the product and our national healthcare ecosystem as the overall total addressable market, that skillful maneuvering is nigh impossible. It’s like trying to turn a cargo ship on a dime. The leaders of a standards committee like HL7 or national exchange network like DirectTrust do not have the luxury of the precise command and control of a normal company. They are constituted of diverse and divergent interests, more often competitors than collaborators, and ensuring uniform adoption is like herding cats.
For Direct, this means expanding into additional use cases has been a slog. Even though it is the clear successor, mainstream markets have been slow to adopt it beyond that initial mandatory use case.
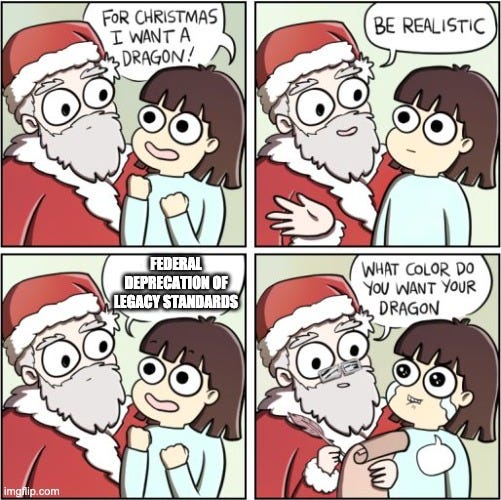
Legislators and regulators are uniquely positioned to help us in crossing the chasm. The right policy could ensure the national adoption of a new standard and end the use of a legacy technology past its prime. Like a product owner, they need to see it through the adoption curve, pushing it beyond the “early adopters” (the specific use cases you define as mandatory), over the chasm, and into all use cases, even ones where the new technology standard is of parity or worse for their purpose. The fastest way to do this is to not to go use case by use case, but to wipe the board - change the problem domain from one saturated with the incumbent solution into one that is essentially whitespace again:


The Dutch approach is not just “you must send via electronic means for X, Y, and Z use cases”. It’s “you must send via electronic means for all health use cases”. It’s a forceful abolishment and deprecation of legacy processes, which functionally necessitates the use (or even creation) of more modern ones. In chasm terms, they’ve wiped the adoption curve clean, launching the legacy technologies of fax and DVD into orbit, like Robin van Persie in the 2014 World Cup.
Holy hell, how refreshingly bold. In some ways, this approach is like a controlled burn. In a dense overgrown forest, you don’t encourage new growth by throwing down seeds and hoping for the best; you remove the cruft in a controlled way, which reduces competition and allows the trees and other foliage you want to grow unrestricted. This also prevents disasters, in that the old buildup is removed. Thinking about our national healthcare ecosystem in this metaphor, we can best allow new technologies to take hold by controlled removal of the lifeless tech of yesterday and create greenfield to allow new technology to take root.
We’ve seen the controlled burn be successful elsewhere before. In 2018, the UK banned the purchasing of new fax machines, with a full ban on any use following in March 2020. There appeared to be some good progress, although post deadline outcomes are handwavy (likely due to COVID taking priority around that time).
Lessons for US
We have a patchwork quilt of legacy technologies in the US, described in this tweet (but also in more detail in Ramps and Rails):

No one from another country would look at this system and think this is the pinnacle of national health technology design. It’s much more akin to “dog sipping coffee in middle of burning room” meme territory. It’s hard to build a holistic solution piecemeal.
It’s because the Dutch approach is not an approach we see in the US often. New technologies have simply slipped into the whitespace - X12 adopted first for the payment cycle, CDA as we realized we needed some basic transfer of patient data between systems, and most recently FHIR for patient authorized exchange. I don’t know what comes after REST, JSON, and OAuth, but I do know that humanity’s penchant for progress means that few technologies last forever. I imagine without change, we’ll see another whitespace filled by the next generation of standards technology, perhaps image exchange or referrals.
In the US, we’ve only notably tried this a few times before, a history that both haunts and informs legislators and regulators as they think towards the future.
Adoption of NCPDP via Meaningful Use
In the late 2000s, there was a standards cold war going on. Electronic prescribing of medications (e-prescribing) had been legalized nationwide in 2007, but there had not yet been ubiquitous adoption of a format. Standards organizations hungrily eyed this new whitespace. Provider healthcare organizations and their EHRs were using primarily HL7v2 to transmit data. However, pharmacies had joined together to form National Council for Prescription Drug Programs (NCPDP) and create their own format - NCPDP SCRIPT. A Yalta conference of sorts was held between the two sides, resulting in an uneasy agreement - a tentative mapping between the two standards.
A single use case with different standards being used by either side is a recipe for disaster. It is hard enough to maintain interoperability with even just a single standard. Thus, it could not last. In 2010, NCPDP struck, lobbying and pushing their standard to be adopted by both hospitals and pharmacies. With the advent of Meaningful Use, NCPDP had won, as HHS required e-prescribing via NCPDP as a core capability of certifying EHRs.
E-prescribing is taken for granted now. It is exceedingly rare to have a paper prescription or even a faxed prescription. However, like Direct, the regulation was entirely too specific. While prescriptions are entirely electronic, other common use cases in pharmacy workflows such as refill status or prescription transfer between pharmacies still rely heavily on fax and phone calls. The job remains unfinished, even with nudges by the CMS to try to iterate a bit.
Adoption of X12 via HIPAA
Going back even further, X12 has existed longer than almost all other standards (you can read more about standards history here). When HIPAA dropped in 1996, lawmakers figured that paper processes between covered entities were no good, so they included a clause that transactions between those parties had to be electronic. Four years later, at the advice of the Workgroup for Electronic Data Interchange (WEDI), the Department of Health and Human Services (HHS) chose that standard to be X12. We’ve barely changed it since - small updates to accommodate new versions of X12 being the main change.
Deprecating paper while requiring X12 at the same time forced the country forward into electronic processing. It’s something people were actually pretty jazzed about, likening it to “the holy grail of practice management”. It’s also a switch that was rightfully viewed as disruptive and possibly expensive. Both perspectives are right and illustrate an important point on how national regulatory policy really does parallel product management.
Improving a core national technical capability is very much akin to a company looking at their tech debt, assessing how their old stack is holding them back, and upgrading that piece of the stack. Ensuring uptime during the switch is challenging and spending resources on that switch disrupts your roadmap. It’s often hard to justify the change instead of working on new capabilities or features.
Looking at the date each dominant technology we use ubiquitously in healthcare came to be and comparing it to a programming language that arose at the same time, our stack is a messy picture. We'd be using COBOL for baseline communication (fax), some C++ to do internal microservices (HL7v2), PHP for payments (X12), .NET to send between instances (CDA), and Swift to do consumer facing functions (FHIR).
The approach we’ve taken has left us spread across disparate standards and the current regulatory push via ONC Cures and CMS Patient Access doesn’t drastically change this. The entropy in the system is only increased by tacking on new formats, but letting old incumbents persist. It’s an administrative burden on organizations that have to support so many standards and it’s a cognitive burden on anyone that wants to enter healthcare and create something new.
Creating whitespace
These two examples show us complementary ideas to keep in mind as we think about ending the fax (or any outdated ubiquitous technology):
Use cases leave exceptions and exceptions leave the job unfinished - NCPDP shows that a subtle, use case defined rollout of a standard is fine and can be effective for piloting technology or limiting scope, but it’s not enough if your goal is elimination of the old standard.
What’s new today will be old tomorrow - The example of X12 shows how new fancy standards can quickly grow stagnant. Cohesive national infrastructure needs to evolve over time to stay modern, so encoding in law into perpetuity or not having a forcing function to re-evaluate these “solved” areas.
The government uniquely possesses the ability to execute in this way, wipe away what is used today, and create the whitespace to allow for quick, unfettered adoption of what we want to be used tomorrow.
What might that tomorrow hold? Personally, like many, I would love to see us move to a FHIR forward future. There’s a particular workgroup, FHIR at Scale Taskforce, focused on this that has outlined many of the components needed for a modern national infrastructure. While as a self-referential acronym, it has arguably the worst nickname of any FHIR workgroup, this to me is the most promising area.
To get there, though, means to displace the baggage of the past. Perhaps a healthcare savvy House rep may read this post and be inspired to bring Axe the Fax to America. Or perhaps a state with solid regional infrastructure like North Carolina might regulate to push the ball forward. Bringing the Dutch approach to the US will be tough, but it will force change.
Barring that, ubiquitous standards and technologies don’t and won’t disappear overnight. Checks and ACH still underpin too much of our financial underbelly, despite fintech and crypto offering superior alternatives. SMS still lurks on as the prevalent standard for messaging, even as Whatsapp and others have distinct advantages. Credit card bureau checks are still the golden standard for identity, even though knowledge-based questions suck and biometrics are way easier.
Current regulatory approach suggests we’ll see similar drawdowns for many things in healthcare. There’s just not much appetite to be that disruptive at scale. Fax will persist and we’ll wonder why. DVDs will persist and we’ll wonder why. HL7v2 will persist and we’ll wonder why.
As for me, I’ll keep daydreaming of chasms, fires, and the Netherlands.
Big shout out to Gabe, Maitreyee, and Ben, a.k.a. the UHWGKOSG (United Healthcare Writer’s Guild of the Kevin O’Leary Slack Group) for their editing. Also to my aforementioned MBA twin Colin for his tweaks.
Edit: Kim Bellard pointed out how Japan has a minister specifically dedicated to Administrative Reform, which is sweet. Can only imagine what we could do here with such a position













I think what you're proposing is actually deregulation. It's removing the regulations that currently artificially prop up the fax machine to create a whitespace. The other reasons as to why the fax machine may still be ubiquitous wouldn't hold up for long if it wasn't for that, just like they didn't in every other non-regulated industry.
I'm not against banning the fax machine, for the record. I simply think it's very risky because what history tells us happens is that using heavy handed regulation to remove something usually ends up with the same heavy handed regulation propping something else up... and that just becomes the new sleepy incumbent. That's when we end up with X12, HL7v2, or the fax in the first place for that matter.